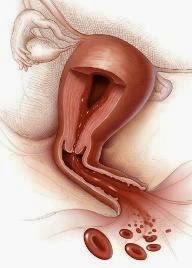
Menorrhagia is term used to describe excessively heavy blood loss during a period (a 'heavy' period).
But, asking the question 'How heavy are your periods?’ is something that doctors know to be unhelpful. This is because what one woman considers acceptable another will find intolerable.
Instead, doctors find that asking ‘How do your periods affect your life?’ is better. For example some women have to change their sanitary protection very frequently and others find that their protection can be overwhelmed by bleeding. Others find that they need to stay at home or take time off from work because of their periods.
So, from a medical point of view, periods that flood or contain clots would be seen as excessively heavy, as would periods that result in anaemia.
So, from a medical point of view, periods that flood or contain clots would be seen as excessively heavy, as would periods that result in anaemia.
Research scientists have calculated that regularly having periods whose total period blood loss is greater than 70 mls can lead to ill health. Therefore this figure has been chosen as the line above which you have officially got menorrhagia, whether or not your periods bother you.
Calculating the volume of blood lost during a period is impractical outside of research laboratories so your doctor will weigh up all your evidence to make the diagnosis.
What Causes Menorrhagia?
Heavy periods can occasionally be caused by medical conditions but, most often, it is just the way the womb happens to work. Heavy periods in the absence of a medical condition are called ‘dysfunctional’ uterine bleeding or DUB for short.
Periods are part of the regular cycle of fertility. The female hormones cause the womb lining to build up so that a fertilised egg can implant and form a pregnancy. Most of the time pregnancy does not occur and the lining has to be disposed of. It is this disposal of the lining tissue that periods are all about.
When a girl first starts to menstruate (and in the last few periods before the menopause in older women ovulation) the release of a egg may not occur. These infertile cycles are associated with different hormone levels to those of fertile cycles. This explains why periods in young girls and older women differ can differ to those of women in their fertile years.
Sometimes heavy periods can be the result of a medical condition. Your doctor will want to consider these if you have period problems.
These Conditions Fall Into Several Groups:
• Tumour; this medical word includes all growths, the vast majority of which are nothing to do with cancers. Fibroids are the commonest of these, although the presence of these swellings of the womb muscle tissue is not necessarily related to heavy periods. Bleeding between periods or bleeding provoked by sexual activity is NOT menorrhagia and should prompt you to see your doctor with some urgency.
• Pregnancy; Do not be surprised if your doctor wants to do a pregnancy test. If nothing else it excludes this cause from further enquiries. Bleeding problems can be caused by early pregnancy events. Rarely cells from the afterbirth can continue growing in the womb after childbirth or miscarriage and cause bleeding. A pregnancy test will detect these cells' presence in the womb, even though the women is not actually pregnant.
• Blood disorders; Very rarely a women may have a blood clotting disorder which can show up with heavy periods. In such cases you may well have had bleeding problems after dental surgery or injury in the past. Please note, this cause is very rare!
• Infection; If there is an infection in the womb the periods can become heavier. In such cases periods may well be painful. Pain with intercourse, lower abdominal tenderness and sometimes (but not always) a vaginal discharge can also occur.
• Psychological factors; Sometimes menstruation can become a focus for anxiety or unhappiness even though the periods are normal. This is a difficult area for your doctor to explore but it is nevertheless important. For some women it appears that periods, although well within what could be called normal, are experienced as intolerable. The various drug treatments tend not to help in such cases. Keeping a period diary and counting items of sanitary wear can be helpful here.
• Other causes include thyroid disorders (very uncommon), a side-effect of certain contraceptives (for example the coil and Depo Provera injections) and excessive body weight.
What Are The Signs And Symptoms Of Menorrhagia?
• Flooding; if the flow of blood with your period overwhelms sanitary towels or tampons then you are flooding.
• Clots; clots signify rapid and heavy blood loss that overwhelms the womb's natural mechanisms that keeps the period in liquid form. This is a sign of heavy bleeding.
• Exhaustion; anaemia can lead to fatigue, but more commonly there appears to be something about periods that induces tiredness - even in women who have normal periods.
• Pain; this is not necessarily associated with heavy periods. Some women with period pain have normal periods and some women with heavy periods have no pain. Your doctor will want to ask about this. Painful periods (known as dysmenorrhoea) are categorised into spasmodic (cramps with the period) or congestive (aching or constant pain usually beginning before the onset of bleeding) types. The type of dysmenorrhoea can point to different causes of menorrhagia.
• Social Problems; a few women experience periods so heavy that, at times, they are confined to the house or even, for a time, confined to the toilet. If your periods are causing social and employment problems you should see your doctor.
Will I Have Any Tests Or Investigations?
• Menstrual calendar; Keep dates and even draw a month-by-month pictorial chart to display your cycle. This helps your doctor and can be very helpful for yourself. Charts help you to control your body rather than it controlling you.
• Physical examination; A general check up may reveal signs of anaemia or thyroid problems. Your doctor will wish to examine your tummy and perform an internal (vaginal) examination. If appropriate, a cervical smear test or swabs for infection might be taken at the same time.
• Blood tests; A blood count for anaemia and measurement of your iron stores is usual. Some women require certain specific tests like thyroid function or hormone tests. Rarely tests of blood clotting are requested.
• Hospital investigations; In addition to physical and vaginal examinations you may be referred to hospital. There, a gynaecologist may suggest looking into your womb with a small telescope (hysteroscope). The gynaecologist may also want to scan your tummy and womb with an ultrasound machine. Some of the newer ultrasound scans can be performed using a probe passed into the vagina to give a very clear picture of the pelvic organs. It goes without saying that no test can be performed on you without your consent. If you are uneasy about what is being advised or do not want a particular test, you should know that the choice is yours. In such circumstances, ignoring your wishes would be wrong
What Treatment Might I Need?
Every woman is different and each woman will have different requirements at different times in her life. For example, hysterectomy for a young woman is unlikely to be appropriate while the contraceptive pill may not be advisable for an older woman. The list of treatments that follows will give you an idea of the options your doctor has available for you.
• Reassurance; The first rule of medicine is ‘primum non nocere’ (first do no harm). If the heaviness of the period is acceptable it is okay to do nothing other than reassure you that no medical treatments are needed at the moment. If your situation changes then a review with your doctor is advisable
• Iron; Iron tablets may be all that you need but more commonly iron is used to replenish deficiency while other treatments are used to ‘turn the tap off’, so to speak. Iron should only be used if a blood test shows that it is deficient. A follow-up test some weeks or months later should be done to monitor the effect of the treatment and to decide when it should be stopped.
What Causes Menorrhagia?
Heavy periods can occasionally be caused by medical conditions but, most often, it is just the way the womb happens to work. Heavy periods in the absence of a medical condition are called ‘dysfunctional’ uterine bleeding or DUB for short.
Periods are part of the regular cycle of fertility. The female hormones cause the womb lining to build up so that a fertilised egg can implant and form a pregnancy. Most of the time pregnancy does not occur and the lining has to be disposed of. It is this disposal of the lining tissue that periods are all about.
When a girl first starts to menstruate (and in the last few periods before the menopause in older women ovulation) the release of a egg may not occur. These infertile cycles are associated with different hormone levels to those of fertile cycles. This explains why periods in young girls and older women differ can differ to those of women in their fertile years.
Sometimes heavy periods can be the result of a medical condition. Your doctor will want to consider these if you have period problems.
These Conditions Fall Into Several Groups:
• Tumour; this medical word includes all growths, the vast majority of which are nothing to do with cancers. Fibroids are the commonest of these, although the presence of these swellings of the womb muscle tissue is not necessarily related to heavy periods. Bleeding between periods or bleeding provoked by sexual activity is NOT menorrhagia and should prompt you to see your doctor with some urgency.
• Pregnancy; Do not be surprised if your doctor wants to do a pregnancy test. If nothing else it excludes this cause from further enquiries. Bleeding problems can be caused by early pregnancy events. Rarely cells from the afterbirth can continue growing in the womb after childbirth or miscarriage and cause bleeding. A pregnancy test will detect these cells' presence in the womb, even though the women is not actually pregnant.
• Blood disorders; Very rarely a women may have a blood clotting disorder which can show up with heavy periods. In such cases you may well have had bleeding problems after dental surgery or injury in the past. Please note, this cause is very rare!
• Infection; If there is an infection in the womb the periods can become heavier. In such cases periods may well be painful. Pain with intercourse, lower abdominal tenderness and sometimes (but not always) a vaginal discharge can also occur.
• Psychological factors; Sometimes menstruation can become a focus for anxiety or unhappiness even though the periods are normal. This is a difficult area for your doctor to explore but it is nevertheless important. For some women it appears that periods, although well within what could be called normal, are experienced as intolerable. The various drug treatments tend not to help in such cases. Keeping a period diary and counting items of sanitary wear can be helpful here.
• Other causes include thyroid disorders (very uncommon), a side-effect of certain contraceptives (for example the coil and Depo Provera injections) and excessive body weight.
What Are The Signs And Symptoms Of Menorrhagia?
• Flooding; if the flow of blood with your period overwhelms sanitary towels or tampons then you are flooding.
• Clots; clots signify rapid and heavy blood loss that overwhelms the womb's natural mechanisms that keeps the period in liquid form. This is a sign of heavy bleeding.
• Exhaustion; anaemia can lead to fatigue, but more commonly there appears to be something about periods that induces tiredness - even in women who have normal periods.
• Pain; this is not necessarily associated with heavy periods. Some women with period pain have normal periods and some women with heavy periods have no pain. Your doctor will want to ask about this. Painful periods (known as dysmenorrhoea) are categorised into spasmodic (cramps with the period) or congestive (aching or constant pain usually beginning before the onset of bleeding) types. The type of dysmenorrhoea can point to different causes of menorrhagia.
• Social Problems; a few women experience periods so heavy that, at times, they are confined to the house or even, for a time, confined to the toilet. If your periods are causing social and employment problems you should see your doctor.
Will I Have Any Tests Or Investigations?
• Menstrual calendar; Keep dates and even draw a month-by-month pictorial chart to display your cycle. This helps your doctor and can be very helpful for yourself. Charts help you to control your body rather than it controlling you.
• Physical examination; A general check up may reveal signs of anaemia or thyroid problems. Your doctor will wish to examine your tummy and perform an internal (vaginal) examination. If appropriate, a cervical smear test or swabs for infection might be taken at the same time.
• Blood tests; A blood count for anaemia and measurement of your iron stores is usual. Some women require certain specific tests like thyroid function or hormone tests. Rarely tests of blood clotting are requested.
• Hospital investigations; In addition to physical and vaginal examinations you may be referred to hospital. There, a gynaecologist may suggest looking into your womb with a small telescope (hysteroscope). The gynaecologist may also want to scan your tummy and womb with an ultrasound machine. Some of the newer ultrasound scans can be performed using a probe passed into the vagina to give a very clear picture of the pelvic organs. It goes without saying that no test can be performed on you without your consent. If you are uneasy about what is being advised or do not want a particular test, you should know that the choice is yours. In such circumstances, ignoring your wishes would be wrong
What Treatment Might I Need?
Every woman is different and each woman will have different requirements at different times in her life. For example, hysterectomy for a young woman is unlikely to be appropriate while the contraceptive pill may not be advisable for an older woman. The list of treatments that follows will give you an idea of the options your doctor has available for you.
• Reassurance; The first rule of medicine is ‘primum non nocere’ (first do no harm). If the heaviness of the period is acceptable it is okay to do nothing other than reassure you that no medical treatments are needed at the moment. If your situation changes then a review with your doctor is advisable
• Iron; Iron tablets may be all that you need but more commonly iron is used to replenish deficiency while other treatments are used to ‘turn the tap off’, so to speak. Iron should only be used if a blood test shows that it is deficient. A follow-up test some weeks or months later should be done to monitor the effect of the treatment and to decide when it should be stopped.
The dose of iron should not be high, no more than one or two tablets a day, because your body can only absorb a small amount each day. Higher doses only increase the risk of side-effects like indigestion or constipation. If your tummy is very sensitive to iron then weaker preparations can be given and your doctor may advise you take just two or three doses per week.
Iron is toxic when taken as an overdose, so keep tablets well away from children. Rarely, iron deficiency can be so great that severe anaemia develops. In such cases blood transfusion in hospital is an option.
• Hormones; Many women find that when they stop taking the combined contraceptive pill (ones with oestrogen and progestogens in them) their light ‘pill periods’ get heavier. The combined pill can be a good option, especially if contraception is wanted as well.
• Hormones; Many women find that when they stop taking the combined contraceptive pill (ones with oestrogen and progestogens in them) their light ‘pill periods’ get heavier. The combined pill can be a good option, especially if contraception is wanted as well.
The traditional use of various progesterone-like drugs has been more or less discredited and, apart from emergency control of a particularly heavy period or to delay a period for social reasons, it is rarely used now. Some women use the high-dose injected contraceptive progestin Depot Provera for cycle control. This, however, is unusual and a non-licensed treatment
• Drugs that affect bleeding and clotting; Normally when blood is released from the body it clots. Period blood is different. Within it are chemicals than break up clots so that the period blood can flow. Heavy bleeding overwhelms this system and result in the passage, sometimes painfully, of clots.
• Drugs that affect bleeding and clotting; Normally when blood is released from the body it clots. Period blood is different. Within it are chemicals than break up clots so that the period blood can flow. Heavy bleeding overwhelms this system and result in the passage, sometimes painfully, of clots.
Drugs that help the clot-dissolving system can dramatically reduce blood loss. Ask your doctor about tranexamic acid. Another drug (ethamsylate) has a similar action but is far less effective.
• Mefenamic acid; This preparation belongs to the class of drugs that includes painkillers and anti-inflammatories like ibuprofen. They work in menorrhagia by blocking the formation of locally acting hormones in the womb called prostaglandins and work best if taken in five-day courses beginning just before the period starts. If pregnancy is a possibility the start should be delayed until the period begins. As with all drugs there are pros and cons. You may have a condition where particular drugs should not be taken
• The Mirena; This intrauterine contraceptive device or coil carries a progesterone-like drug into the womb. It lasts for five years and, unlike the copper coils, actually reduces the heaviness of the period. Although it has not yet got a licence for treatment of menorrhagia it is being used increasingly for this purpose, especially if contraception is required as well. It can be an alternative to hysterectomy in some women
• Anti-hormones; There are drugs that can switch off the hormone and egg production of the ovary. They are commonly used in hi-tech fertility treatments and in certain gynaecological conditions. However, although the ‘GnRH’ group of drugs will stop periods, they have little place in the management of menorrhagia and no place in general practice medicine
• Endometrial ablation; If you have completed your family, techniques to permanently remove the lining tissues of the womb can be very effective in treating heavy periods. It can be an alternative to hysterectomy and can be performed as a day case procedure. Ablation is a medical word meaning ‘destroy’. If the lining is destroyed then it may not be possible to carry a pregnancy afterwards. However the procedure is not the same as a sterilisation so contraceptive precautions should be thought about. Note: endometrial ablation doesn’t work for everyone
• Hysterectomy; Removing the womb removes periods and any chance of pregnancy. Hysterectomy is a frequently performed, but fairly major, operation. Most women opting for this will have tried a range of less drastic options. In some cases, however, hysterectomy can help with other problems too (for example sterilisation, fibroids and period pain). Hysterectomy must be discussed carefully with your doctor and your gynaecologist.
What Course Will The Illness Follow?
If the heaviness of your periods is in the range that constitutes menorrhagia then treatment is advisable. In the absence of treatment a woman with menorrhagia will develop anaemia, which can result in the gradual appearance of fatigue, tiredness, pallor and even breathlessness.
• Mefenamic acid; This preparation belongs to the class of drugs that includes painkillers and anti-inflammatories like ibuprofen. They work in menorrhagia by blocking the formation of locally acting hormones in the womb called prostaglandins and work best if taken in five-day courses beginning just before the period starts. If pregnancy is a possibility the start should be delayed until the period begins. As with all drugs there are pros and cons. You may have a condition where particular drugs should not be taken
• The Mirena; This intrauterine contraceptive device or coil carries a progesterone-like drug into the womb. It lasts for five years and, unlike the copper coils, actually reduces the heaviness of the period. Although it has not yet got a licence for treatment of menorrhagia it is being used increasingly for this purpose, especially if contraception is required as well. It can be an alternative to hysterectomy in some women
• Anti-hormones; There are drugs that can switch off the hormone and egg production of the ovary. They are commonly used in hi-tech fertility treatments and in certain gynaecological conditions. However, although the ‘GnRH’ group of drugs will stop periods, they have little place in the management of menorrhagia and no place in general practice medicine
• Endometrial ablation; If you have completed your family, techniques to permanently remove the lining tissues of the womb can be very effective in treating heavy periods. It can be an alternative to hysterectomy and can be performed as a day case procedure. Ablation is a medical word meaning ‘destroy’. If the lining is destroyed then it may not be possible to carry a pregnancy afterwards. However the procedure is not the same as a sterilisation so contraceptive precautions should be thought about. Note: endometrial ablation doesn’t work for everyone
• Hysterectomy; Removing the womb removes periods and any chance of pregnancy. Hysterectomy is a frequently performed, but fairly major, operation. Most women opting for this will have tried a range of less drastic options. In some cases, however, hysterectomy can help with other problems too (for example sterilisation, fibroids and period pain). Hysterectomy must be discussed carefully with your doctor and your gynaecologist.
What Course Will The Illness Follow?
If the heaviness of your periods is in the range that constitutes menorrhagia then treatment is advisable. In the absence of treatment a woman with menorrhagia will develop anaemia, which can result in the gradual appearance of fatigue, tiredness, pallor and even breathlessness.
Anaemia can also affect health generally and so recovery from coughs and colds may be slower. In reality very few women will tolerate menorrhagia long enough for severe anaemia to develop.
Can I Do Anything To Help Myself?
Unfortunately there is nothing much you can do to make your periods lighter or heavier, or to change their frequency, unless you consider using one of the treatments listed above. It is a good idea to keep a note of your period dates and perhaps a calendar of their duration, heaviness and whether you have clots or other symptoms like pain.
Tell Your Doctor
1. The dates when your last few periods began. The regularity or otherwise of your periods is important information.
2. Your doctor may ask about how heavily your sanitary wear (towels and tampons) are affected by your periods. Some doctors use a chart that can be used to estimate the amount of blood lost by counting how many items are used and how heavily they are stained. The presence of clots or flooding is important.
3. Be prepared to be asked whether you have bleeding between periods or after intercourse. Your doctor may also want to know when your last cervical smear test was done and what the result was.
4. Your doctor may want to know about any previous pregnancies you may have had and, importantly, if you want children in the future. Your current and future (if any) contraception may need to be considered in order to choose the best treatment for you.
5. Your doctor may want to know how you are generally in yourself and perhaps details of your diet, if it is unusual. If you have other symptoms, be prepared to mention them as they may point to treatable causes of your period problem.
Ask Your Doctor
1. What precisely is the best way to take medications like mefenamic acid or tranexamic acid in order to reduce the period? These are important questions as these drugs only work if they are taken as a short course.
2. Is there anything to suggest that my heavy periods could be part of another disorder? Although most women with menorrhagia simply have a womb that is programmed to give them heavy periods, sometimes heavy periods are caused by other conditions, for example fibroids, pelvic infection or endometriosis.
3. Is there anything to suggest that the heavy periods are compromising my health? The answer will almost certainly be no. However it would not be unusual if your doctor thought it necessary to check your blood count or, perhaps, your body’s iron stores. If there were evidence of any other problems your doctor would want to allow them up too.
4. Should I be referred on to a gynaecologist? In most cases your own GP will be able to investigate and treat you for menorrhagia. Referral on to a gynaecologist would only be required if there was evidence of another gynaecological disorder or if your doctor considered you may be a candidate for operative treatments like hysterectomy or endometrial ablation.
5. Would the Mirena coil be a suitable choice for my problem? At the present time the Mirena only has a license for contraception. However it is being used increasingly to control heavy periods, even in women who do not require contraception. There is no consensus of opinion about this question at the moment, but it is one worth asking. After all, if having a Mirena coil fitted controls your periods and means you do not have to consider hysterectomy then it is valid to ask questions about it.
Useful Contacts
Women's Health
Address: 52 Featherstone Street, London, EC1Y 8RT
Telephone: (+44) 07092 228194
Fax: 0207 608 0928
Helpline: 0207 251 6580
Contact Name: Danny Tucker
Email: editor@womens-health.co.uk
Website: www.womens-health.co.uk
Can I Do Anything To Help Myself?
Unfortunately there is nothing much you can do to make your periods lighter or heavier, or to change their frequency, unless you consider using one of the treatments listed above. It is a good idea to keep a note of your period dates and perhaps a calendar of their duration, heaviness and whether you have clots or other symptoms like pain.
Tell Your Doctor
1. The dates when your last few periods began. The regularity or otherwise of your periods is important information.
2. Your doctor may ask about how heavily your sanitary wear (towels and tampons) are affected by your periods. Some doctors use a chart that can be used to estimate the amount of blood lost by counting how many items are used and how heavily they are stained. The presence of clots or flooding is important.
3. Be prepared to be asked whether you have bleeding between periods or after intercourse. Your doctor may also want to know when your last cervical smear test was done and what the result was.
4. Your doctor may want to know about any previous pregnancies you may have had and, importantly, if you want children in the future. Your current and future (if any) contraception may need to be considered in order to choose the best treatment for you.
5. Your doctor may want to know how you are generally in yourself and perhaps details of your diet, if it is unusual. If you have other symptoms, be prepared to mention them as they may point to treatable causes of your period problem.
Ask Your Doctor
1. What precisely is the best way to take medications like mefenamic acid or tranexamic acid in order to reduce the period? These are important questions as these drugs only work if they are taken as a short course.
2. Is there anything to suggest that my heavy periods could be part of another disorder? Although most women with menorrhagia simply have a womb that is programmed to give them heavy periods, sometimes heavy periods are caused by other conditions, for example fibroids, pelvic infection or endometriosis.
3. Is there anything to suggest that the heavy periods are compromising my health? The answer will almost certainly be no. However it would not be unusual if your doctor thought it necessary to check your blood count or, perhaps, your body’s iron stores. If there were evidence of any other problems your doctor would want to allow them up too.
4. Should I be referred on to a gynaecologist? In most cases your own GP will be able to investigate and treat you for menorrhagia. Referral on to a gynaecologist would only be required if there was evidence of another gynaecological disorder or if your doctor considered you may be a candidate for operative treatments like hysterectomy or endometrial ablation.
5. Would the Mirena coil be a suitable choice for my problem? At the present time the Mirena only has a license for contraception. However it is being used increasingly to control heavy periods, even in women who do not require contraception. There is no consensus of opinion about this question at the moment, but it is one worth asking. After all, if having a Mirena coil fitted controls your periods and means you do not have to consider hysterectomy then it is valid to ask questions about it.
Useful Contacts
Women's Health
Address: 52 Featherstone Street, London, EC1Y 8RT
Telephone: (+44) 07092 228194
Fax: 0207 608 0928
Helpline: 0207 251 6580
Contact Name: Danny Tucker
Email: editor@womens-health.co.uk
Website: www.womens-health.co.uk

















No comments:
Post a Comment